Advocating With Rare Disease: Communication Strategies for Lipid Storage Disorders
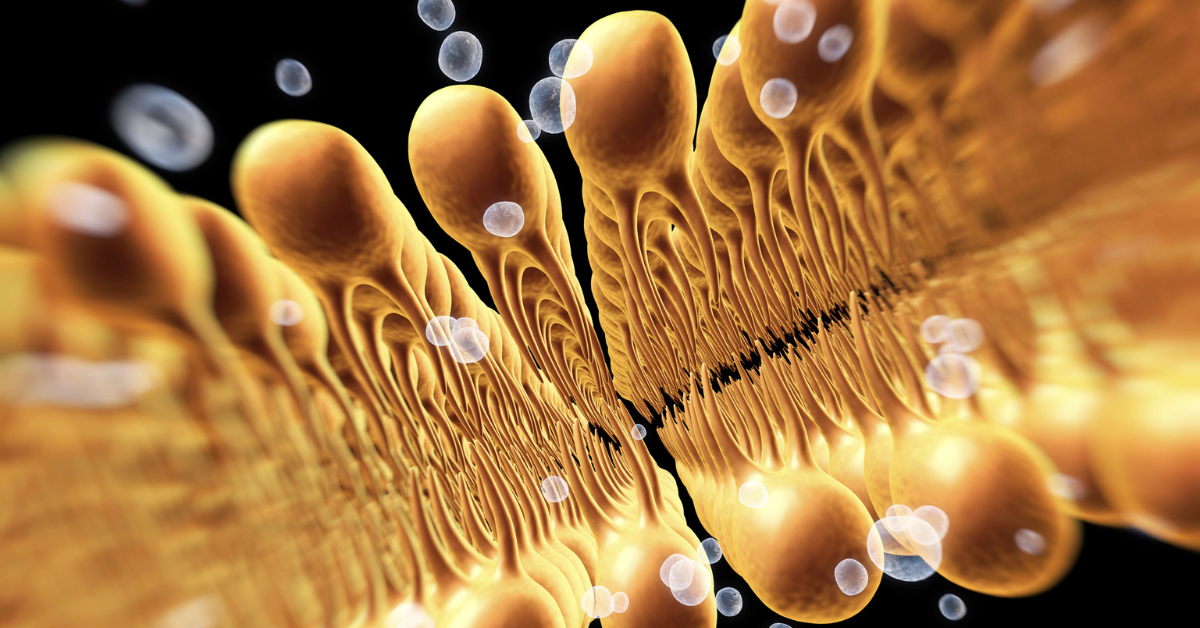
Living with a lipid storage disorder means navigating a healthcare system where most providers have limited experience with your condition. Whether you have Gaucher disease, Fabry disease, Niemann-Pick, or another lysosomal storage disorder, you face unique challenges: explaining complex genetics to new providers, coordinating between multiple specialists, and advocating for treatments that many doctors have never prescribed. Understanding how to communicate about your rare disease effectively can transform your healthcare experience from frustrating to collaborative.
Why this matters in real appointments
Lipid storage disorders affect fewer than 10,000 people in the United States combined, with Gaucher disease affecting approximately 1 in 40,000 to 1 in 60,000 people and Fabry disease affecting 1 in 40,000 to 1 in 120,000¹. This rarity creates specific communication challenges. Emergency room physicians might never have encountered your condition. New specialists might confuse symptoms with more common conditions. Even well-meaning providers might make assumptions based on outdated information from medical school rather than current treatment protocols.
The multi-system nature of these conditions adds complexity. Gaucher disease can affect the spleen, liver, bones, and blood, while Fabry disease impacts the kidneys, heart, nervous system, and skin². This means you’re often coordinating between hematologists, geneticists, cardiologists, nephrologists, neurologists, and primary care providers who may not regularly communicate with each other. Each specialist might focus on their organ system without seeing the bigger picture of your overall disease management.
The evolution of treatments makes advocacy even more critical. Enzyme replacement therapies (ERT) like imiglucerase for Gaucher disease and agalsidase for Fabry disease have transformed outcomes³, but not all providers are familiar with these treatments or their monitoring requirements. Newer options like substrate reduction therapy and chaperone therapy require even more specialized knowledge⁴. You often become the expert educating your care team about emerging treatments and current best practices.
Practical strategies you can use today
-
Create a one-page disease primer for new providers: Develop a concise summary that explains your specific condition, current treatments, and key monitoring needs. Include your specific genetic mutation if known, as this can affect disease severity and treatment response.
Include in your primer: “I have Type 1 Gaucher disease (specific mutation: L444P/L444P). This is a lysosomal storage disorder causing glucocerebroside accumulation. I receive bi-weekly enzyme replacement therapy with imiglucerase. Key monitoring includes: CBC for thrombocytopenia, chitotriosidase levels for disease activity, and annual MRI for bone involvement. My treating specialist is Dr. [Name] at [Institution], phone: [number].”
-
Use the “teaching moment” approach with unfamiliar providers: When encountering providers unfamiliar with your condition, position yourself as a collaborative educator rather than a challenging patient.
Try saying: “I know Fabry disease is quite rare, so you might not see it often. The key things relevant to today’s visit are that it causes neuropathic pain and can affect kidney function. I have some recent specialty notes that might be helpful for context. Would you like me to highlight the most relevant parts for what we’re discussing today?”
-
Bridge the specialty gap with explicit connection requests: Don’t assume your specialists are communicating. Actively request and facilitate information sharing between providers.
Try saying: “My nephrologist recently adjusted my ACE inhibitor dose due to proteinuria from my Fabry disease. Since cardiac involvement is also common in Fabry, could you please review this change and coordinate with them? I can sign a release for direct communication if that would help. Here’s their direct line and the best times to reach them.”
-
Document symptom patterns specific to your condition: Track symptoms in the context of your disease’s known patterns, helping providers distinguish disease progression from unrelated issues.
Try documenting: “Pain crisis began 3 days ago, consistent with my typical Fabry-related acroparesthesia pattern: burning in hands and feet, triggered by temperature change, not relieved by standard analgesics. Different from my usual pattern: location now includes forearms. Using my prescribed gabapentin with partial relief. Previous similar episodes have responded to IV hydration and climate control.”
Navigate emergency and urgent care situations
Emergency departments present unique challenges for rare disease patients. Create an emergency protocol letter from your specialist that you can present immediately upon arrival. This should include your diagnosis, current treatments, medications to avoid, and specific complications to watch for. For example, patients with Gaucher disease should have documentation about bleeding risk due to thrombocytopenia, while those with Fabry disease need alerts about renal function and cardiac considerations.
When presenting to emergency care, lead with both your acute concern and your underlying condition: “I have chest pain that started two hours ago. I have Fabry disease, which can cause cardiac complications. My cardiologist is Dr. [Name] at [Institution].” Bring your medication list including your specialty infusions, as emergency providers may not be familiar with enzyme replacement therapy protocols or may need to verify that certain medications won’t interfere with your treatment.
Coordinate complex treatment logistics
Managing enzyme replacement therapy or other specialized treatments requires significant advocacy. Insurance prior authorizations for medications costing hundreds of thousands of dollars annually require detailed documentation. Work with your specialty pharmacy coordinator and maintain your own records of authorization numbers, approval dates, and renewal requirements. Create calendar reminders for reauthorization submissions at least 60 days before expiration.
If you receive infusions, advocate for consistency in your care setting. Request the same nurses when possible, as they become familiar with your specific needs and reaction patterns. Document any adverse reactions meticulously, including pre-medication effectiveness and infusion rate tolerances. This documentation becomes crucial if you need to change infusion centers or if insurance questions the medical necessity of specific protocols.
Build your rare disease communication toolkit
Develop different “elevator pitches” for your condition based on the audience and situation. For a new primary care provider, focus on overall health maintenance and red flags. For a specialist, emphasize organ-specific manifestations relevant to their expertise. For insurance representatives, use precise medical terminology and billing codes. Having these prepared statements reduces emotional labor and ensures consistent, accurate communication.
Consider creating a portable medical record binder or digital folder containing: recent genetic testing results, baseline organ function studies, treatment history timeline, specialist contact information, and published treatment guidelines for your condition. Many providers appreciate having access to current guidelines from sources like the National Gaucher Foundation or Fabry Support and Information Group, as these may be more recent than their reference materials.
Address genetic and family planning conversations
Lipid storage disorders’ genetic nature means you’ll need strategies for discussing inheritance patterns, family screening, and reproductive planning. When discussing family screening, be prepared for providers who may not understand the inheritance patterns. For X-linked conditions like Fabry disease, female carriers can have significant symptoms despite older literature suggesting they’re asymptomatic⁵. Advocate for appropriate screening and treatment for affected family members regardless of gender.
For reproductive planning discussions, come prepared with specific questions and resources. Know your mutation type and what genetic counseling options are available. If a provider dismisses concerns with outdated information, respond with current data: “Recent studies show that female carriers of Fabry disease can have significant organ involvement. Given this, what monitoring would you recommend during pregnancy?” Having citations ready can help shift the conversation from dismissal to collaborative planning.
Connect with specialty centers and research opportunities
Advocate for referrals to centers of excellence for your condition. The National Institutes of Health maintains a list of specialized centers for lysosomal storage disorders. These centers offer multidisciplinary clinics where you can see multiple specialists in coordinated visits. When requesting referrals, emphasize the efficiency and comprehensive care these centers provide: “The lysosomal storage disorder center at [Institution] has a multidisciplinary clinic where I can see all my specialists in one day. This would reduce my travel burden and improve care coordination.”
Stay informed about clinical trials and emerging treatments through patient organizations and ClinicalTrials.gov. When discussing research participation with your providers, frame it as part of comprehensive care: “I’m interested in contributing to research that might help others with my condition. Are you aware of any studies I might qualify for, or could you connect me with someone involved in lysosomal storage disorder research?” This positions you as an engaged patient while potentially accessing cutting-edge treatments.
Make it stick this week
- Create or update your one-page disease primer with current treatment information and specialist contacts.
- Draft an emergency protocol letter template and request your specialist’s signature at your next appointment.
- Set up a medical binder or digital folder with your key documents, organized by category.
- Research if there’s a center of excellence for your condition within reasonable travel distance.
- Join at least one patient organization for your specific condition to stay informed about treatment advances.
Living with a lipid storage disorder means becoming an expert in your own condition and an educator for your healthcare team. While this shouldn’t be necessary, it’s the current reality of rare disease care. By developing strong communication strategies, maintaining comprehensive documentation, and building collaborative relationships with providers, you can create a care team that truly understands and effectively manages your condition. Remember, your lived experience with your rare disease is valuable expertise that deserves respect and consideration in every healthcare interaction.
References:
1. Mehta A, Winchester B, eds. Lysosomal Storage Disorders: A Practical Guide. Wiley-Blackwell; 2012.
2. Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5:30.
3. Stirnemann J, Belmatoug N, Camou F, et al. A Review of Gaucher Disease Pathophysiology, Clinical Presentation and Treatments. Int J Mol Sci. 2017;18(2):441.
4. Schiffmann R, Hughes DA, Linthorst GE, et al. Screening, diagnosis, and management of patients with Fabry disease: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int. 2017;91(2):284-293.
5. Wilcox WR, Oliveira JP, Hopkin RJ, et al. Females with Fabry disease frequently have major organ involvement: lessons from the Fabry Registry. Mol Genet Metab. 2008;93(2):112-128.
Disclaimer: This article provides general information about communication and advocacy. It is not medical or legal advice. Consult a qualified professional for guidance on your specific situation.
